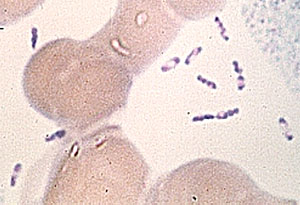
Image courtesy of neiljs; CC-BY 2.0 DEED.
As of December 5th, 17 people in the Kyotera district of Uganda have died of what has now been confirmed to be anthrax [1]. Tests initially ruled out anthrax, along with Marbug, Ebola, Crimean Congo Hemorrhagic Fever, and the Rift Valley Fever; however, according to the Uganda daily news, Monitor, the Kyotera District Health Officer confirmed that samples from the cases tested positive for anthrax on November 26th [1,2,3]. Animals in the area have also been dying, which led medics to initially believe the mysterious outbreak was caused by anthrax. Anthrax is not contagious, but someone can be infected if they come in contact with infected animals or animal products [4]. The WHO recommended that villagers refrain from consuming deceased animals to prevent anthrax infection. [1]. The media reports anywhere from 28-40 cases have been identified. Cases have presented with fever and rashes, and some have swollen limbs [5].
Anthrax, caused by the bacterium Bacillus anthracis, is prevalent in regions such as Central and South America, sub-Saharan Africa, and central and southwestern Asia. The transmission of anthrax is commonly linked to domestic and wild animals, including livestock and deer, who become infected by ingesting or inhaling spores from contaminated soil, plants, or water. Human susceptibility to anthrax increases when handling the carcasses of infected animals [4]. Anthrax manifests in three primary forms with distinct routes of entry into the body. Cutaneous anthrax, the most frequent and least dangerous form, occurs when spores enter the body through the skin, often through cuts or wounds. While most patients recover with proper treatment, untreated cases have a 20% fatality rate. Inhalation anthrax, caused by breathing in spores, is the most lethal, with nearly all untreated cases leading to fatalities, but aggressive treatment increases survival to approximately 55%. Gastrointestinal anthrax arises from consuming raw or undercooked meat from an infected animal, and proper treatment yields a 60% survival rate, dropping to over 50% without treatment. Recently, a fourth type of anthrax, injection anthrax, has been discovered in heroin-injecting drug users in northern Europe. This type of anthrax is similar to cutaneous anthrax but can be harder to recognize and treat [4].
Anthrax spores live in soil underneath vegetation, where they are protected from sunlight. However, Uganda is vulnerable to heavy rain and flooding that erode the land and force livestock to graze closer to the soil, introducing them to anthrax spores [6,7]. Farmers, faced with economic constraints, may be reluctant to euthanize sick animals. Climate change, along with no incentives to report or cull ill animals, has increased Ugandans’ risk of anthrax [7].
The anthrax outbreak in Uganda underscores the critical intersection of environmental factors, climate change, and livestock management practices in amplifying the risk of anthrax transmission. The confirmed cases highlight the urgent need for comprehensive public health measures, emphasizing both accurate diagnostics and community cooperation in preventing the spread of the disease. Mitigating the impact of anthrax in Uganda requires a holistic approach, addressing not only immediate health concerns but also environmental sustainability and climate resilience. As the nation grapples with this outbreak, lessons learned can inform future strategies, emphasizing the imperative of proactive and collaborative efforts to safeguard public health in the face of emerging infectious threats.
Sources:
- https://www.monitor.co.ug/uganda/news/national/anthrax-outbreak-kyotera-death-toll-now-rises-to-17-4448800
- https://www.monitor.co.ug/uganda/news/national/12-killed-as-strange-disease-hits-kyotera-4440736
- https://www.monitor.co.ug/uganda/news/national/more-cases-recorded-as-kyotera-strange-disease-puzzles-medics-4443826
- https://www.cdc.gov/anthrax/basics/index.html#:~:text=People%20can%20get%20sick%20with,like%20the%20cold%20or%20flu.
- https://www.youtube.com/watch?v=sOEr7cMzFug
- https://www.cnn.com/2022/09/08/africa/uganda-heavy-rain-climate-intl/index.html#:~:text=After%20a%20prolonged%20drought%2C%20heavy,Mbale%20district%20in%20eastern%20Uganda.
- https://www.seattletimes.com/sponsored/climate-change-linked-to-rise-in-infectious-diseases/