By: Alexandra Rodrigues and Autumn Gertz
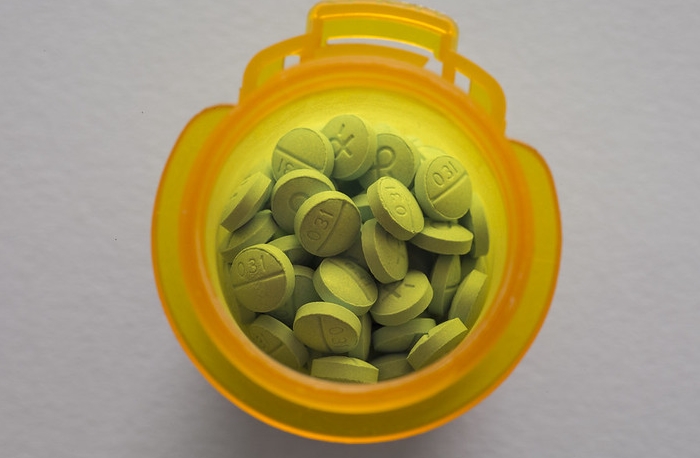
Image courtesy of Quote Catalog via Flickr
While life before COVID-19 may serve as many people’s standard of normalcy, for millions of Americans struggling with substance use disorders (SUD), it was a daily battle. In 2018, approximately 20.3 million Americans aged 12 or older had a SUD related to alcohol or illicit drug use, in the past year [1]. Of those people, roughly 8.1 million had an illicit drug use disorder [1]. The overshadowed SUD epidemic at stake involves opioid misuse, which is defined as the use of heroin or the misuse of prescription pain relievers [1]. Overdosing on opioids is common due to the strong potency of the drugs and their tendency to be laced with stronger, cheaper drugs such as fentanyl, making this disorder especially deadly.
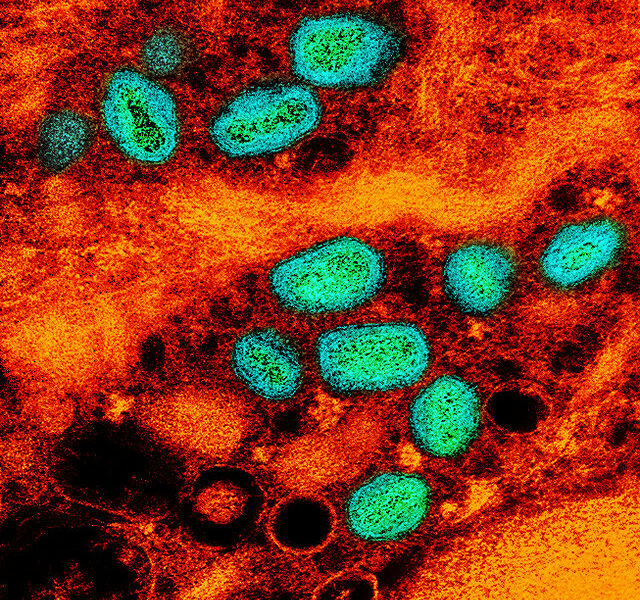
The COVID-19 pandemic has led to an increase in fatalities from overdosing according to Dr. Anahi Ortiz, a Coroner in Franklin County, Ohio who said in August, “there’s been a 65% increase in overdose fatalities for the first six months of 2020 compared to the first six months of 2019” [2]. One possible explanation for this increase is the disruption of drug trafficking due to COVID-19, making it harder to buy certain drugs, tempting people to start creating their own drug concoctions despite not knowing the potency of what they are mixing [3]. Isolation and record-breaking unemployment rates create the perfect conditions for the development and exacerbation of mental health issues. Approximately 1 in 4 people with a serious mental illness such as major depression, also have a SUD [4]. It is possible people turn to alcohol and illicit drug use as a form of self-medication, in order to “treat” their mental illness [4].
Before the pandemic, thousands of Americans turned to methadone and suboxone maintenance centers as a starting point to sobriety. Methadone and Suboxone are drugs that prevent substance users from going into withdrawal from opioid use, without getting them high [5]. Since the pandemic began, many of these centers have been forced to close or limit their hours of operation, leaving people scrambling to find their “fix”, even if that means relapsing. Some had to travel hours each morning to reach the closest clinic. While the weather was warm, some clinics were able to remain open and operate outdoors. The winter has had a devastating impact on those who depend on those clinics, with the cold weather forcing some to temporarily close. Fortunately, the Substance Abuse and Mental Health Services Administration (SAMHSA) has given providers working in an Opioid Treatment Program (OTP), the authorization to dispense methadone based on telehealth appointments, rather than an in-person appointment [6]. They are allowed to dispense 14 doses for clinically less stable patients and 28 doses for clinically stable patients; clinical stability is determined by the provider and the patient’s medical record [6]. This is a much-needed step in the right direction to combat the catastrophic impact COVID has had on the growing opioid crisis.
References
[1] https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHNatio…
[2] https://abc6onyourside.com/news/local/increase-in-bodies-sent-to-franklin-county-morgue-in-2020