It seems logical to think that over diagnosing an illness would not bring too much harm – better safe than sorry, right? Wrong. A study, published recently in the British Medical Journal, shows that there is a serious problem with over diagnosing malaria in Afghanistan, and the impacts are significantly negative.
Adding to the body of research done on misdiagnosis of malaria in other parts of the world, researchers from the London School of Hygiene and Tropical Medicine and Afghanistan-based research organizations looked at 22 primary care clinics in two Afghan provinces to see what proportion of patients suspected of having malaria were accurately treated. They compared diagnoses and treatment outlined in 2357 patients’ records to blood samples and found that many of the patients had tested negative for the parasite, yet were still being treated.
The problem with this, the researchers said, is that serious non-malarial illnesses go untreated, malaria drugs are wasted, and the cost effectiveness of the malaria diagnostic tests is reduced.
According to the World Health Organization guidelines on malaria and malaria treatment, wherever and whenever it is possible, parasitological diagnosis is recommended. However, this can only be done through microscopy and rapid diagnostic tests- methods that may not be available in all settings.
In areas without lab equipment, clinicians from the study relied on signs and symptoms to diagnose patients with a fever. Malaria symptoms are non-specific, meaning that they are symptoms not just of malaria, but of other illnesses as well. The WHO recommends that in settings with a low prevalence and risk of malaria, diagnosis should be based on fever within the past three days and possibility of exposure to malaria. In settings where malaria is endemic, diagnosis is based on fever within the past 24 hours, and signs of anemia. All diagnoses should be confirmed with parasitological tests.
According to the study, of 415 patients diagnosed with malaria based on symptoms, 412 were actually negative, and had been given malaria medication anyway. Only one percent was diagnosed and treated accurately (meaning the patients had malaria and were treated for malaria). In contrast, in that same clinic, a second group was diagnosed using microscopy. From this group, 63 percent (127/202) was diagnosed and treated accurately. An improvement, but that still means that 37 percent of that population received malaria medication without being infected.
Why would clinicians give malaria drugs to patients with negative test results? Authors of the study looked to research done in Tanzania and Ghana for possible explanations. One factor was a perception that malaria was more prevalent in the area than it actually was – a belief that could be further perpetuated by continual over-diagnosis of the parasite. Others included a lack of confidence in the negative lab result or limited access to treatments for other febrile illnesses.
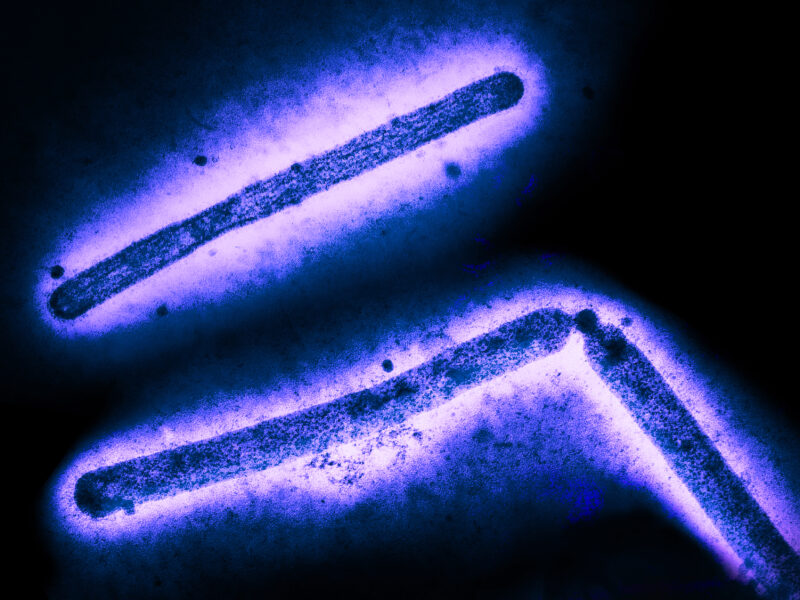
While malaria is endemic in Afghanistan, it is less prevalent than in other parts of the world. Plasmodium falciparum, the most deadly type of malaria, exists in the region, but it is extremely rare. The far more dominant subtype in Afghanistan, Plasmodium vivax, is less dangerous. If a patient presents with fever, the cause could be malaria, but it is also likely to be a viral or bacterial infection. If it is a viral or bacterial infection, but the patient is treated for malaria, the non-malarial infection can worsen.
As the researchers suggested, mistreatment with malaria medication also poses the risk that the parasite will develop a resistance to treatment. As the Disease Daily reported earlier this year, there is evidence of artemisinin-resistant malaria popping up along the Thailand-Myanmar border.
Studies have shown that introducing rapid malaria tests in areas without access to microscopes significantly reduces oversubscription of malaria medication and leads to better targeting of antibiotics.
But rapid tests alone may not be enough to eliminate misdiagnosis. Even when diagnoses were right, there is evidence of providing medication when it was not needed. All clinicians in the study were to follow a standard set of guidelines. Those guidelines, however, were somewhat ambiguous when defining “confirmed” versus “suspected” cases or “clinical” malaria, and erred on the side of precaution. Better training and clearer guidelines for clinicians are needed in order to reduce risk for drug resistance, missed treatment opportunities, and misdiagnosis of febrile illness.
The study’s authors state that the findings are likely to be representative of many parts of Afghanistan and possibly other countries in south and central Asia.
“Until widespread misdiagnosis and treatment has been corroborated in other countries it is impossible to be sure that it is representative of south and central Asia in general,” stated the authors, “but our view is that it is safer to assume that it is and to take robust steps to identify and tackle what is likely to be a major public health challenge.”