Image courtesy of Michael Wunderli on Flickr, CC
Human African trypanosomiasis (HAT), also known as sleeping sickness, is a potentially fatal neglected tropical disease.1 The recent approval of a new drug treatment has the potential to play a significant role in efforts to eliminate the disease. On November 16, 2018, the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) approved the use of fexinidazole to treat sleeping sickness.2 It was recommended under Article 58, which allows CHMP to evaluate and provide opinions on drugs and vaccines that are intended for use outside the European Union.2,3 Fexinidazole is expected to make treatment of sleeping sickness much easier, as it is the first treatment of the disease in pill form.2
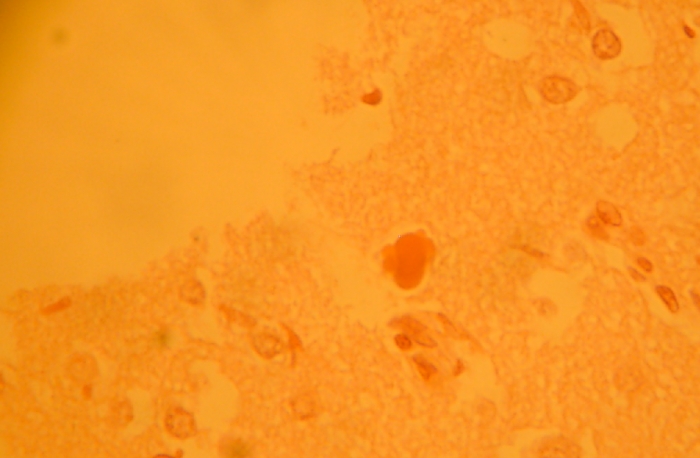
Human African trypanosomiasis is caused by an infection by one of two subspecies of parasite: Trypanosoma brucei gambiense or Trypanosoma brucei rhodesiense. The trypanosome is transmitted to humans when they are bitten by a tsetse fly.1 In some instances, a fetus can become infected if the parasite crosses the placenta. HAT is most common in rural areas, where exposure to tsetse flies is greatest.
Sleeping sickness has two stages. In the first stage, called the haemo-lymphatic stage, the parasites multiply in subcutaneous tissues, blood, and lymph.1 Some of the common symptoms of this stage include fever, headaches, joint pain, and itching. The subsequent/second stage, called the neurological or meningo-encephalic stage, is much more severe, as the parasite has crossed the blood brain barrier, infecting the central nervous system. The disease derives its name from the disruption of the sleep cycle that often occurs in this stage of the disease.4 Other symptoms include aggression, confusion, poor coordination, and psychosis.1,4 If the disease is left untreated, the patient is likely to die within two to three years of infection.2
There are two types of parasites that cause the disease.1 Approximately 97% of HAT cases are caused by Trypanosoma brucei gambiense, which is found in 24 countries in west and central Africa. People who have been infected by this type may go months or years without any symptoms. However, by the time any obvious symptoms emerge, most people are already in the second stage of the disease. The other type is Trypanosoma brucei rhodesiense, which is found in 13 countries in eastern and southern Africa. T.b. rhodesiense is more virulent and progresses more rapidly than Gambian trypanosomiasis.5 The infection typically progresses from the incubation period to the haemo-lymphatic and neurological stages within weeks. Some patients may experience septic shock and multi-organ failure within days of the initial development of a fever.
In 2017, the World Health Organization (WHO) recorded a total of 1,447 cases of HAT, with 1,420 T.b. gambiense cases, and 27 T.b. rhodesiense cases.6,7 The majority of cases (76%) occurred in the Democratic Republic of Congo (DRC), which is the only country that continues to report at least 1,000 cases to WHO each year.1,6 The country with the second greatest number of cases, Guinea, reported only 140 cases in 2017.6
Prior to the approval of fexinidazole, there were five drug treatments available for sleeping sickness. The first stage of T.b. gambiense infection is typically treated with an intravenous infusion or intramuscular injection of pentamidine, while the first stage of T.b. rhodesiense infection is treated with suramin.8 One of the earliest treatments for the second stage of both types of infection was melarsoprol, an arsenic derivative.1 Melarsoprol has some serious potential side effects, including phlebitis and reactive encephalopathy, which is fatal in 3-10% of cases.1,8 In some areas, the parasites are also showing increased resistance to malarsoprol.8 Unfortunately, it remains the only effective treatment for second stage T.b. rhodesiense infection. Second stage T.b. gambiense infection can be treated with eflornithine, and in 2009, a nifurtimox-eflornithine combination therapy was introduced. The combination treatment reduces the duration of treatment and the amount of eflornithine needed, but still consists of a week of twice daily intravenous infusions of eflornithine in combination with nifurtimox pills.1,9
In 2005, the Drugs for Neglected Diseases initiative (DNDi) rediscovered “fexinidazole”, a drug originally developed in the 1970s by the German drug company, Hoechst (now merged with Sanofi) as a broad-spectrum antiparasitic drug4,10 The drug had been shelved, but in 2009, DNDi entered into an agreement with Sanofi to develop, manufacture and distribute it.4
Recent clinical trials of fexinidazole conducted with 749 patients in the DRC and Central African Republic have found the drug to have “high efficacy and safety” in both stages of HAT caused by T.b. gambiense, in adults and children older than six years who weigh at least 20 kilograms.4 In a randomized, phase two/three trial, fexinidazole cured 91% of people with second stage disease, compared to 98% treated with combination therapy.9,11 This cure rate was considered to be within the acceptable margin of 13% for difference in success rates.11 Fexinidazole also cured 99% of people with early stage disease.9
Fexinidazole is expected to greatly reduce the difficulty of treating sleeping sickness.4 Rather than intravenous infusions, patients will only have to take a once daily pill for 10 days. In addition, as the drug is able to cure both stages of the disease, only a blood test will be required to confirm the presence of the disease, rather than a lumbar puncture to determine disease stage.12 As a result, more people will have access to treatment, as it reduces the need for hospitalization.4 A trial is currently underway to test if fexinidazole is appropriate for home administration.11 The drug is currently expected to be available for distribution in endemic countries in 2019.12 Sanofi is donating the drug to WHO, which distributes sleeping sickness drugs for free to endemic countries.1,4
Sources:
- http://www.who.int/news-room/fact-sheets/detail/trypanosomiasis-human-african-(sleeping-sickness)
- https://www.ema.europa.eu/en/news/chmp-recommends-first-oral-only-treatm…
- https://www.ema.europa.eu/en/human-regulatory/marketing-authorisation/medicines-use-outside-european-union
- https://www.dndi.org/2018/media-centre/press-releases/ema-recommends-fexinidazole-first-all-oral-treatment-sleeping-sickness/
- http://www.antimicrobe.org/b54.asp
- http://apps.who.int/gho/data/node.main.A1636?lang=en
- http://apps.who.int/gho/data/node.main.A1637?lang=en
- https://www.cdc.gov/parasites/sleepingsickness/health_professionals/index.html
- https://www.nature.com/news/sleeping-sickness-can-now-be-cured-with-pills-1.22856
- Pollastri M. Fexinidazole: a new drug for African sleeping sickness on the horizon. Trends in Parasitology. 2018; 34(3): 178-179. https://doi.org/10.1016/j.pt.2017.12.002
- Mesu VKBK, Kalonji WM, Bardonneau C, et al. Oral fexinidazole for late-stage African Trypanosoma brucei gambiense trypanosomiasis: a pivotal multicentre, randomised, non-inferiority trial. Lancet. 2018; 391: 144-54. http://dx.doi.org/10.1016/S0140-6736(17)32758-7
- https://www.npr.org/sections/goatsandsoda/2018/11/16/668623229/sleeping-…