By: Elisa Cink and Kelsey Sweeney
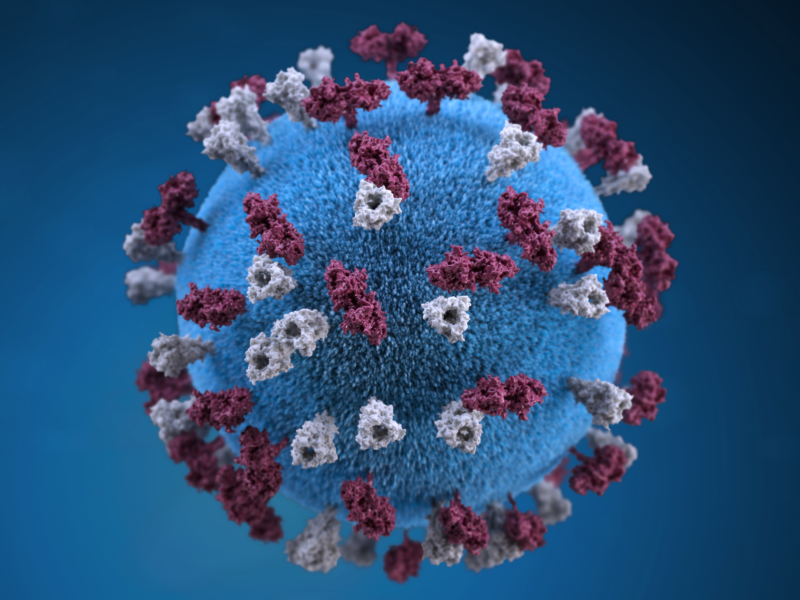
Image courtesy of Tim Green; CC-BY.
H5N1 avian flu, also known as bird flu, is a highly infectious viral disease that primarily affects birds. Throughout history the virus has been found in over 60 countries all over the world and has been responsible for infection and mortality in humans and a variety of mammals.1 H5N1 is once again making headlines for variant emergence and transmission in mammals. Public health researchers have growing concerns that the bird flu virus will mutate to a form that is highly transmissible and pathogenic among humans to create the next pandemic.2
Avian influenza A viruses can be classified into two categories: highly pathogenic and low pathogenic and refer to the severity of disease in infected animals. However, both forms of the virus can cause severe disease in humans.3 Highly pathogenic avian influenza H5N1 virus was first identified in domestic waterfowl (a goose) in 1996 in Southern China. In 1997, poultry outbreaks occurred in China and Hong Kong, where the virus was transmitted to humans for the first known time, leading to 18 cases and 6 deaths in Hong Kong.1 Since the first human outbreak, H5N1 has gone on to infect over 870 people resulting in an estimated 457 deaths (Case Fatality Rate (CFR) over 50%) in 21 different countries.4
Avian influenza pandemics have made their devastating imprint in public health history, and officials recognize the need to monitor both animal outbreaks and human cases to prevent the next pandemic. Under the International Health Regulations (IHR 2005) Article 6, Member States are required to report information on every case of H5N1 human infection or novel influenza virus infection to the World Health Organization (WHO).5 The WHO maintains a record of all human cases over the past 20 years.6 The HealthMap platform at Boston Children’s Hospital helps to monitor emerging threats and provides early warning and situational awareness to the public health community; since the beginning of 2023, HealthMap has captured over 560 relevant articles for avian influenza event tracking.7
So far, the transmission of the H5N1 virus from person-to-person has been very rare, limited, and not sustained.8 In 2006, an outbreak in Indonesia resulted in 162 cases and 134 deaths in humans (CFR 83%).9 Between 2003-2019, Egypt faced 392 cases of H5N1 with a 34% CFR. Egypt is one of the few countries where H5N1 virus has become enzootic, though the reason for the high number of human cases has not been identified.10 More recently, there have been sporadically reported cases of H5N1 in humans. In January 2023, a nine-year-old girl in Ecuador contracted the virus from backyard poultry and was hospitalized for severe symptoms.11 Then, in February 2023, an eleven-year-old girl in Cambodia died from H5N1 after suspected exposure to infected birds/poultry; her father was also infected, but recovered.12,13A woman in China was also diagnosed with H5N1 in March 2023.14 Public health experts suspect most human cases are due to exposure to infected poultry/birds or contaminated environment. Human cases will continue to emerge at the human-animal interface where these avian influenza circulates in animals.15
Currently, there is a worldwide outbreak of H5N1 that is affecting animals. The World Organization for Animal Health reported that H5N1 has killed more than 200 million birds since the beginning of 2021, due to disease and mass culling to curb spread.16 HealthMap previously reported on the affected poultry population and subsequent egg shortage in the United States.4 In February 2023, Peru reported the death of over 63,000 wild birds and 716 sea lions (marine mammals) since November 2022.17,18 Chile reported the country’s first bird flu case in a marine mammal, a sea lion.18 There was also an outbreak at a mink farm in Spain, where over 50,000 minks (which are semi-aquatic mammals) died of H5N1.19 Add these animals to the growing list that are testing positive for H5N1 all over the world including otters, foxes, raccoons, and bears.20 Small mammals share the same basic physiology as humans and can process the virus quickly and facilitate changes in its genetic makeup.21 This is concerning public health experts because the virus is transmissible among different species; however further research is needed to understand virulence and transmissibility of the virus.4
Eradication of the H5N1 virus is challenging, for many reasons including the regular prevalence in poultry, a main food source and employment industry worldwide. For decades, farmers have controlled H5N1 by mass culling of infected animals; however this is not logistically or economically sustainable. And while vaccines are available for poultry/birds, they present challenges. For example, vaccinated birds may test positive for the virus – so farmers cannot guarantee a bird is free of infection, impacting food security, trade, exports, and livelihoods. Also, administering vaccines to wild birds and animals is untenable, so it is very difficult to reduce transmission among wild birds and animals or animals to humans.22 For humans, potential drugs and vaccines exist and could be evaluated as countermeasures should a human outbreak start; non-pharmaceutical interventions, including face masks, education and community engagement, may also help to protect the population.21 Stay up to date on the current H5N1 outbreak by following HealthMap alerts.
References
21. Virtual Press conference on global health issues transcript – 8 February 2023. Accessed March 17, 2023. https://www.who.int/publications/m/item/virtual-press-conference-on-global-health-issues-transcript—8-february-202322. Murray CJ, Ikuta KS, Sharara F, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet. 2022;399(10325):629-655. doi:10.1016/S0140-6736(21)02724-0