Image courtesy of United Nations via Flickr Creative Commons
The current Ebola outbreak in the Democratic Republic of the Congo (DRC) began in 2018 and has affected over 3,000 lives. As of November 12, there have been 3,287 Ebola cases (3,169 confirmed and 118 probable) resulting in 2,193 deaths. This current outbreak is the second largest in history, following the 2014-2016 Western Africa outbreak that claimed over 11,000 lives. Despite this, the current outbreak has led to new developments regarding Ebolavirus and Ebola disease. Two of these new developments are detailed in this article.
Concerning Ebola Case
The WHO and Congolese authorities are searching for answers as the circumstances around a woman’s death remain unclear and contradict widely accepted beliefs about Ebola. The woman in question was working in the “Red Zone” of an Ebola treatment center in Beni prior to falling ill [1]. The “Red Zone” is where patients are quarantined when their illness is severe [1]. She died in July after becoming infected with Ebola for the second time [1]. As she was previously infected with Ebola, it was believed she had immunity to the disease.
The theory of presumed immunity is commonly accepted in regard to Ebola survivors, meaning they cannot become infected again after a prior Ebola infection [1]. This assumption has led many Ebola survivors to work with current patients, as they can provide human contact, something missing for those suffering from the disease [1]. The woman in this case was working primarily with children suffering from Ebola [1]. Janet Diaz, the leader of the World Health Organization (WHO) clinical management team for the Congolese outbreak stated “That was a big red flag event for all of us” [1]. Current procedures for Ebola survivors working with patients are being reconsidered by the WHO and Congolese authorities as a result of this case [1].
There is some speculation that the woman’s original Ebola infection was a false diagnosis, though this has not been confirmed [1]. Additionally, there is more thought arising that Ebola survivors have “incomplete immunity” to Ebola [1]. Therefore, they could be susceptible to further infection. Until more is learned, procedures for Ebola survivors will be adapted to match standard procedures of those working with sick patients, and more restrictions will be put in place regarding which treatment centers survivors can work at [1].
India Spillover of Filoviruses
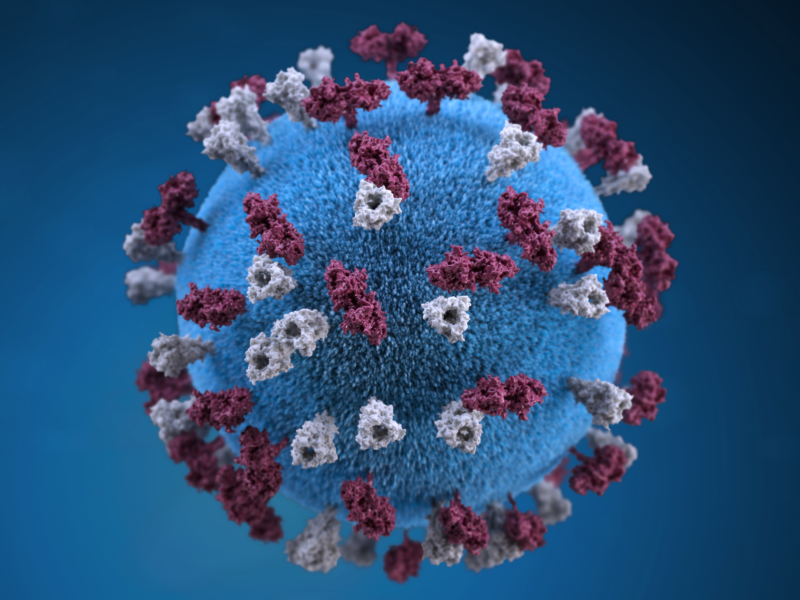
An article published on October 31, 2019 in PLOS Neglected Tropical Disease found that bats and humans in northeast India have evidence of filovirus exposure, the class of virus that causes Ebola [2]. This is the first indication of exposure (via antibody detection) in this region [2]. Northeast India has no history of Ebola disease of hemorrhagic fever [2]. Outbreak News Today also shared the findings of this study [3].
Currently, there are four types of Filovirus known: Ebolavirus, Marburgvirus, Cuevavirus, and Dianlovirus [2]. Within the genus Ebolavirus are Ebola virus, Bundibugyo virus, Taï forest virus, Sudan virus, Reston virus, and Bombali virus [2]. Bats are known reservoirs of filoviruses, and have been suspected as a possible zoonotic transfer in the West African outbreaks of Ebola [2]. Northeast India has a high risk of zoonotic disease transfer from bats to humans as bats are widely hunted and up to 167 species are consumed in this, and surrounding, areas [2].
Blood and serum samples from humans and two bat species (E.spelaes and R. leschenaultiii) were collected in 2017 and analyzed for antibody reactivity to all types of filovirus [2]. Filovirus antibodies were found in 5.9% of humans, 6.2% of E.spelaes bats, and 13.3% of R. leschenaultiii bats[2]. In humans, the antibodies indicated exposure to two genera of filo virus, Marburgvirus and Ebolavirus [2]. Within Ebolavirus, antibodies were detected for Ebola virus, Bundibugyo virus, and Sudan virus [2]. Between the two bat species, Ebolavirus and the recently discovered Mengla virus were detected [2]. The investigators also noted that cross reactivity between filoviruses is similar to previously reported levels and no viral genetic material was found in humans or bats [2].
As Ebola concerns continue globally, it is striking to find evidence of exposure in a region with no history of the disease. The investigators of this study indicate some potential protective barrier to zoonotic transfer that may help to explain why no disease has been recorded in the region. These barriers in include ecological barriers to zoonotic transmission, that viruses are unable to sustain transmission to humans, or that an uncharacterized type of non-pathogenic filovirus, or antigenically related virus, exists in this region [2].
References
[2] https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0007733
[3] http://outbreaknewstoday.com/india-spillover-bats-and-humans-carry-antibodies-to-filoviruses-20517/